
Despite progress with immunotherapy and targeted agents, treatment of refractory disease remains challenging, in particular for patients with T-ALL. Identification of genomic lesions defining actionable targets had limited impact on patient care so far. The complexity of biological systems highlights the need to develop complementary functional approaches. We and others have established platforms with a library of 120 drugs based on current treatment and (pre-)clinical development, to detect ex-vivo drug response phenotypes on leukemia samples at single cell resolution by high content image analysis. We demonstrated that drug response profiling (DRP) identifies dependencies not predicted by genetic alterations adding a functional information layer for clinicians. Here we report first correlations with clinical outcome using DRP in a non-interventional setting.
From 2016 to 2019 we performed DRP in the framework of European ALL first- and second- line protocols upon request by treating centers. Here we analyze retrospectively treatment decisions and outcome for 23 T- and 50 BCP-ALL patients. To evaluate drug responses, we compared dose response curves of individual patients to data recorded for all patients. Sensitivity and resistance were defined based on the IC50 outlier analysis using cut-offs depending on distribution (normal gaussian vs. skewed). From 73 patients tested, clinical outcome data has been available for 36 BCP- and 15 T-ALL patients. NGS data provided by the INFORM registry has been available in 8 BCP- and 2 T-ALL patients.
In first line BCP-ALL patients, ex-vivo Dexamethasone response predicted clinical response to prephase prednisone (d8) and minimal residual disease (MRD) reduction measured by flow cytometry at d15 of first line AIEOP BFM 2009 induction (Fig. 1).
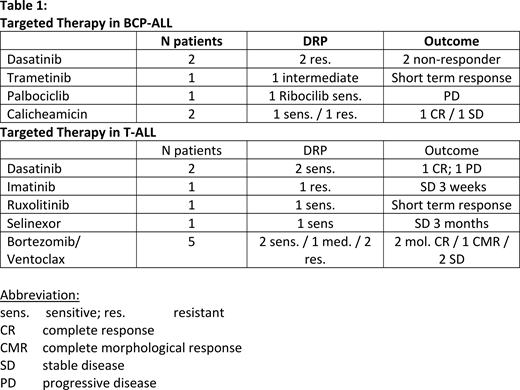
For refractory and relapsed ALL we observed an association of DRP and response to targeted agents in 14 out of 16 patients (87.5 %; Table 1).
Data for the r/r BCP-ALL cohort is limited because most patients underwent CD19 and / or CD22-directed immunotherapy. Sensitivity and resistance to Calicheamicin correlated with clinical response to Inotuzumab, suggesting functional testing to be evaluated in future studies. In contrast, lack of correlation of ex-vivo sensitivity to MEK-inhibitors with presence of RAS-pathway alterations caution the exclusive use of molecular information to predict response to these agents.
Most therapeutic decisions based on DRP information were made for patients with r/r T-ALL. Bortezomib ex-vivo sensitivity correlated with clinical responses in 5 T-ALL patients (Fig. 2). Both patients predicted to respond to Bortezomib and treated on Bortezomib + Venetoclax experienced good MRD response providing a bridge to stem cell transplantation (SCT). However, these patients relapsed after SCT emphasizing the need for additional consolidative therapeutic elements for heavily pretreated patients.
In line with previous reports, we confirmed a T-ALL with high sensitivity to Dasatinib (IC50 1.9 nM; Fig. 3). Dasatinib monotherapy induced a molecular remission. A 2nd T-ALL showing an ex- vivo Dasatinib IC50 at 80 nM was refractory to treatment with Dasatinib + Daunoxome-FLAG. A 3rd ABL1-fusion positive T-ALL, ex-vivo resistant to Imatinib and Dasatinib, had only short- term response to Imatinib + chemotherapy.
Finally, treating a T-ALL patient based on high sensitivity to the XPO1 inhibitor Selinexor as 4th line monotherapy led to significant decrease of PB blasts from d1 25 G/L to 0.7 G/L at d13 of treatment (Fig. 4). The patient experienced improved quality of life, minimizing need of hospitalization with stable disease for 3 months on maintenance with Selinexor. Given the promising preclinical data with this class of agents and current lack of established biomarkers, we propose that DRP should be evaluated for this class of agents.
In conclusion, we established first associations between DRP and clinical response for various agents providing a rationale for the evaluation of DRP in prospective clinical trials. Integration of molecular and functional information may improve the selection of more specific treatment options for patients with resistant disease. The international BFM Study Group and ITCC Consortium are planning an international multiarm early clinical trial for treatment of r/r ALL patients that will include DRP for evaluation in order to improve selection of targeted therapy.
Cario:Jazz Pharmaceuticals: Consultancy, Other: travel support; Novartis: Consultancy, Other: travel support. Hrusak:Amgen: Other: MRD investigations funded by Amgen, Research Funding. Kulozik:Novartis: Consultancy, Honoraria; bluebird bio, Inc.: Consultancy, Honoraria. von Stackelberg:Morphosys: Membership on an entity's Board of Directors or advisory committees, Other: Personal fees, advisory committees and speakers bureau, Speakers Bureau; Roche: Membership on an entity's Board of Directors or advisory committees, Other: Personal fees, advisory committees and speakers bureau, Speakers Bureau; Jazz: Membership on an entity's Board of Directors or advisory committees, Other: Personal fees, advisory committees and speakers bureau, Speakers Bureau; Amgen: Membership on an entity's Board of Directors or advisory committees, Other: Personal fees, advisory committees and speakers bureau, Speakers Bureau; Shire: Membership on an entity's Board of Directors or advisory committees, Other: Personal fees, advisory committees and speakers bureau, Speakers Bureau. Jacoby:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Lonza: Membership on an entity's Board of Directors or advisory committees. Bourquin:Servier: Other: Travel Support.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal